What is Trauma and how does it affect day to day function?
What if your everyday looked and felt like this:
This blog is personal. Not only as an occupational therapist but as a parent. I am the adoptive parent of a child who experienced developmental trauma. Trauma impacted my child and therefore has impacted our family in a profound way. I am grateful that our experience has led me to a new path of understanding. Whether you are the tired parent who feels like everyday is a struggle or the teacher of a student who constantly acts out in the classroom or a friend of someone impacted by trauma, please read on. Understanding that relationship is the treatment may be the key you are looking for.
It is common to hear the term “trauma informed care” these days. Thankfully, many schools, therapists, teachers and even law enforcement agencies are becoming aware of the need for change in how we interact with individuals who have experienced adverse circumstances in their life. It is easy to write off this discussion because you don’t think it applies to you.
But I want to challenge you to continue reading and lean in because the principles discussed in this article not only apply to those who have experienced adversity, but apply to any human who experiences stress on their system. And if you have been on earth during the Covid-19 pandemic - you have experienced Collective Trauma (any traumatic event experienced by a group of people such as war, social injustice or a pandemic). Some of us responded with resilience and some of us have been rattled. Read on to get more insight.
how do you define Trauma?
Needless to say, no child should have to experience circumstances defined as trauma. Unfortunately, it is all too common. While I wish I had a magic wand to end violence, systemic racism, economic disparities, neglect and abuse, I do not. But, we. as individuals and communities who serve children, do have the ability to positively influence children on a daily basis. As Dr. Bruce Perry, renowned child psychologist and expert on trauma, says, “People not programs, change people.”
“The way we experience the world in our minds, bodies and senses, past and present, profoundly impacts our lived experience.”
There is hardly an area of function that isn’t impacted when a child experiences trauma. Functional changes can be seen in emotional, behavioral, cognitive, social and physical aspects of daily life.
The way we experience the world in our minds, bodies, and senses, past and present, profoundly impacts our lived experience.
To put this in practical terms, the ability to function on a daily basis is the outcome of our mind and body connection - which is influenced by past and present sensory experiences, attachment relationships, physical abilities and exposure to stressors.
What is trauma?
When you hear the word “trauma,” what comes to mind?
Physical, emotional and sexual abuse. Domestic violence. Natural Disasters. These are a few of the things that immediately come to mind at the mention of the word “trauma.” These experiences , commonly referred to as Big T traumas, can have a lifetime of consequences for individuals who experience them.
Other types of trauma, called little t traumas, may not be life threatening but can have long lasting impacts on the brain of a child. Developmental trauma is considered to be any traumatic alteration of one’s developing brain, including such things as fetal alcohol syndrome and sensory processing disorder. Other things in this category include neglect, rejection, foster care, adoption, long term hospitalizations and death of a parent. According to Bessel van der Kolk, author of The Body Keeps the Score, the time from conception to age 2 or 3, during which essential brain development occurs, a child’s brain is particularly susceptible to chemicals produced by stress. Complex Trauma arises from repeated exposure to traumatic events or stressors during developmentally vulnerable times in a child’s life.
Definitions can be limiting and the bottom line is that exposure to any of these situations can significantly impact a person’s daily life. Kim Barthel, occupational therapist, recently stated on the Safe and Sound Protocol Podcast, that trauma is an individualized response to a situation - what may be traumatic for one person may not be traumatic to another.
The key takeaway is that diagnoses and labels are not the focus, but what we need to pay attention to is a person’s responses.
Trauma and the Brain
In my previous blog on Seeing Behavior through a New Lens, I explained how our nervous system is set up to detect threats. In this way it protects a person from harm and sets them up for connection. We are social beings and operate best when we are primed and ready to connect. When a traumatic event or stressor enters into the situation the nervous system shifts its responses.
While a full explanation of the neuroscience related to development and trauma is beyond the scope of this blog, it is essential to have some understanding of the fundamental concepts of brain development in order to better understand how trauma and chronic stress can impact function. Hang in there - I will try and keep this information as simple as possible.
In a nutshell, the job of the brain is to take in information from outside and inside the body (from the senses and internal organs) and make sense of it. It does this by making associations between patterns of input that happen together repeatedly.
Key Concepts In Understanding How Trauma Affects the Brain
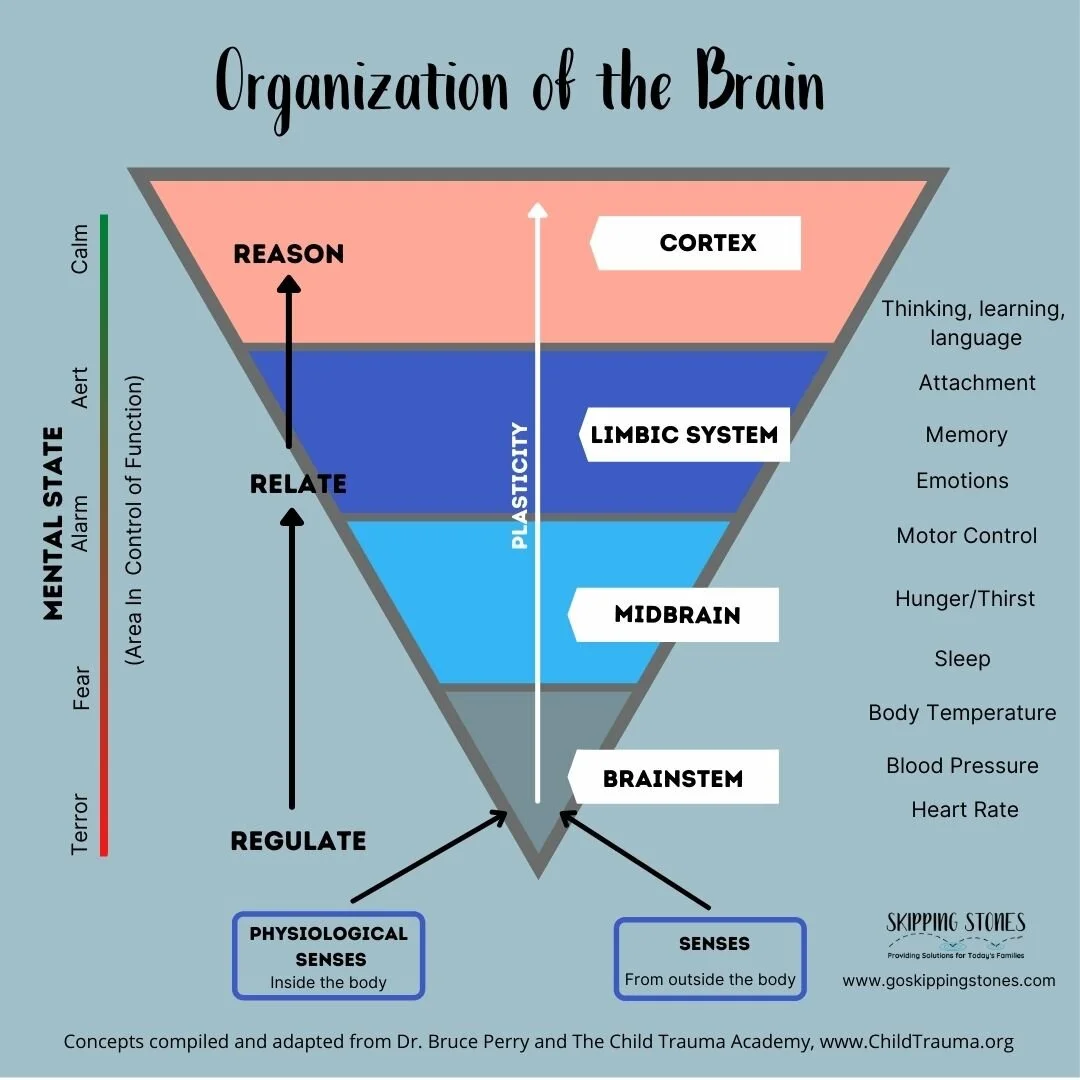
Hierarchy of the brain - According to the neuro-sequential theory of development, the brain is organized in a hierarchical fashion and develops from birth through adolescence in this order: 1. Brain stem and mid brain (sensory and motor control) 2. Limbic System (attachment and emotions) 3. Cortex (thinking, planning, inhibiting, learning.
Co-Regulation - Development takes place in the context of relationships. When a child is born they rely on a caregiver to help them regulate their bodies and their states of arousal. In a healthy environment, through that relationship, a child learns to increase control of their output (behavior) from the brainstem to the thinking part of the brain.
State Dependent Function - Constant monitoring of the environment is how a person perceives threats. Keeping safe is the ultimate goal. Depending on the level of threat, the brain activates different parts of the brain. If threat is perceived as high, the brainstem takes over and responds in an immediate way, without conscious thought. We call this fight/flight or freeze. Dan Siegel refers to this as “flipping your lid.” (See here for a video description.) If the body is in a calm state, access to higher levels of brain activity become available.
Window of Tolerance - We all have a window of tolerance for our nervous system in which we can operate without disrupting normal functioning. When the nervous system can not keep in check the mechanisms that keep this in balance, we flip our lid. Various experiences (i.e. trauma, fear) or physiological states (i.e. hunger, thirst) can impact the width of our tolerance window.
A note about stressors - Not all stressors are bad. By definition, a stressor is simply anything that puts a demand on our body outside of normal capabilities. Stress is essential to healthy development and is an essential ingredient in building resilience. According to Dr, Bruce Perry, important factors that establish whether a stressor will produce increased resilience or vulnerability are whether it is predictable, moderate or controllable.
Putting It All Together
When a child experiences trauma or chronic stress, their brains are continually in a state of fear putting them in fight/ flight or freeze mode even when they are in a safe environment. Not only is this correlated with poor long-term health, it puts them in a state of alarm, which makes it near impossible to access the thinking part of their brain. The implications of this are huge.
Because connection and attachment happen above the brainstem level, it is very difficult for children who are stuck at this level to form secure attachments. Not only this, but because of the way the brain connects sensory input and facial recognition, a child may have distorted interpretations of non verbal cues resulting from associations made during unsafe, distorted interactions with others in past experiences.
Managing emotions and behavior is a challenge, as well. Common practices of thinking and reflection are ineffective. Because the child is stuck in fear mode, it is difficult to access the cortex of the brain for academic learning. While a child may be intelligent, they just can’t learn. They may appear angry, oppositional or shut down and withdrawn. Feelings of failure can create low self-esteem or lead to depression.
Knowing where a child is developmentally or how old they were when they began experiencing trauma is essential to healing. Because the brain develops from the bottom up, it may be necessary to approach a child from their developmental age as opposed to their chronological age.
Thankfully, there is hope. Because the brain is malleable and can change with experience in the context of loving and caring relationships, children who have experienced trauma can heal. Depending on the age of the child and their neurological strengths, change may take time. The essential thing to remember is that connection must come first.
Some children who have experienced trauma may experience challenges in their ability to process sensations. For a detailed look at all the sensory systems you can read my earlier blog. It is important to note, however, that some children who have not experienced Big T trauma, face sensory challenges on a daily basis. This may put their body in a state of high arousal or fear on a daily basis. Outward behaviors may appear similar in the classroom. No matter the cause or the diagnosis, a neurodevelopmental approach is needed to organize and integrate all levels of the brain.
An occupational therapist, trained to help children address sensory processing challenges can help children function more effectively on a daily basis by looking at a child’s sensory processing systems and seeing where the challenges are. Through clinical skill and reasoning, the OT can help a child experience sensations in a new way so that they can meaningfully interact at home, in the classroom and in the community.
If you need more help or feel like your child needs the help of a professional, please contact someone in your area for support. You can start with your pediatrician or ask around for the name of a counselor who is right for you. An occupational therapist who is knowledgeable about trauma can support your family by helping find solutions to your everyday challenges.
Stay tuned for more practical ways to help the children in your life who have been impacted by trauma.