A new paradigm for approaching behavior
Your child’s behavior is driving you crazy!
Rewards don’t work. Reasoning doesn’t work. Yelling doesn’t work. Now what?
Until recently behavior was only seen as an act of the will - something a child chooses to do. But recent discoveries in neuroscience show that behavior stems from responses way below the conscious level in the central nervous system. The drive to avoid threat and remain safe is what drives behavior.
A person’s brain is constantly checking (4 times/second) to know if their body is safe. Without the feeling of safety, a person is unable to connect socially and is unable to engage the part of the brain that can make rational decisions.
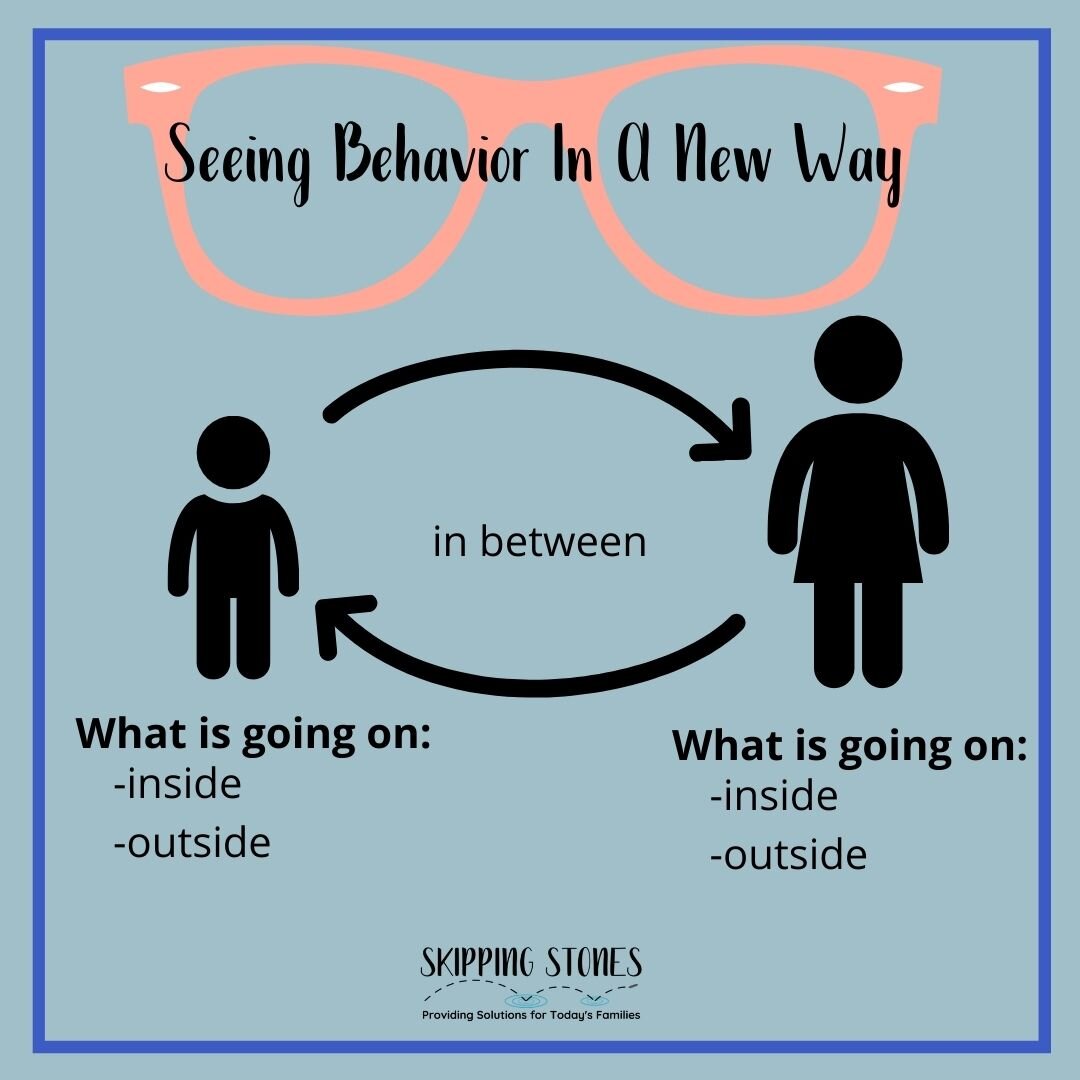
This “felt safety” is about perceived safety not literal safety. “Felt safety” is a subjective experience (unique to an individual) that is a result of a person’s internal experiences, relationships (caregiver and others) and their environment. Deb Dana, author of Rhythm and Regulation, regards its this way: responses are a result of everything inside, outside and in between.
(Throughout this blog I will be referring to the behavior of a child, but this information is true for all humans. Robyn Gobbel often refers to this approach as being human-informed.)
What this means is that more often than not, a child will respond to a situation in a way that is familiar to their body in order to protect themselves. To put it another way, your child is doing the best that they can, in the moment, with the skills that they have, to keep themselves safe.
Does this mean it is the best way to respond? NO! Does it mean it is the most appropriate way to respond? NO! And because most responses happen below a conscious level, they are not fully aware of why they are doing what they are doing.
Our job as caregivers is to show up for them and through connection, help them feel safe in their bodies and learn how to engage their thinking brain to manage their responses. To do that we need to see what is going on below the surface.
I can hear you saying, “Wait, wait, wait! My child is totally safe. They have a family, they go to school, they have three meals a day and a roof over their head. What is this about safety?”
I am glad you asked! This shift in perspective about behavior is going to take some time to process. Any shift in thinking takes adjustment. For me, it was an “Aha!” moment that helped me understand my own neuro-diverse child. I hope you will hang in there and give it a chance. It can guide you in a new understanding of your child, a child in your sphere of influence or perhaps, yourself.
I have taken many classes and seminars on this approach and there is a lot to learn but I will try to break it down into its basic elements.
First, a few guiding principles to understanding this approach to behavior:
Principle # 1: The Autonomic Nervous System protects the body through management of Energy and arousal levels
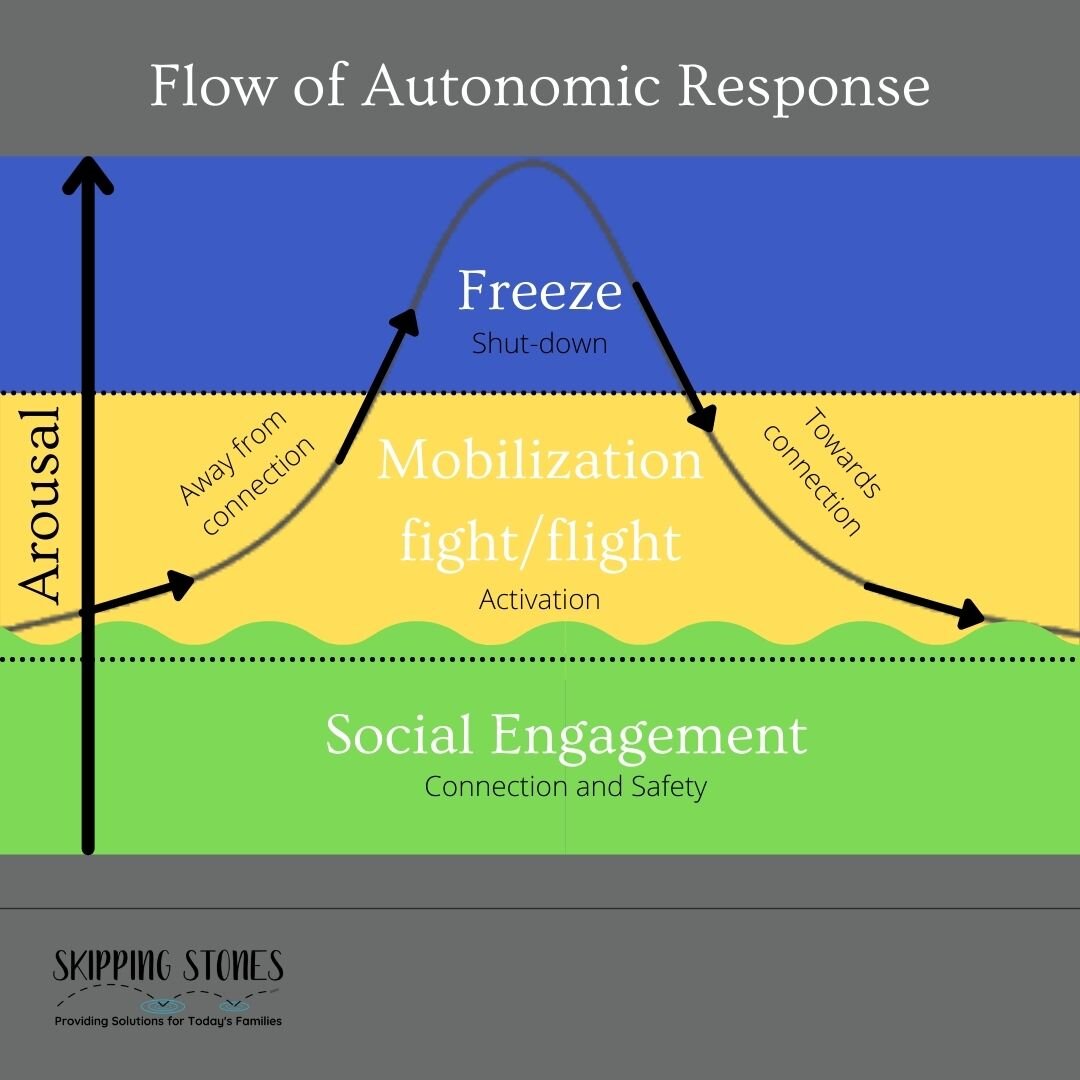
The autonomic nervous system is the system in the body that controls automatic body functions (heart rate, breathing, blood pressure, digestion, etc.), survival responses and social engagement. This system of sensory input and motor output controls all of these essential functions without us having to think about them. The job of the autonomic nervous system is to keep the body safe through control of energy and arousal levels.
Three pathways of the autonomic nervous system operate sequentially to respond to situations in the environment. The body constantly moves through these pathways throughout the day. A ventral vagal pathway is ready for connection and social engagement, feels safe and is emotionally regulated and can access higher thinking skills.
If a threat is perceived, the sympathetic pathway is activated and readies the body for action. In this stressed state, the thinking brain goes “offline” and a response look like a meltdown, a tantrum or even excessive silliness.
If completely overwhelmed, the body move to a dorsal vagal pathway. Here, withdrawal and shut down are the key components. The body slows down, eyes gaze downward, shoulders slump in an effort to conserve energy. Sometimes overlooked as quiet compliance, this state can be missed as a cry for help.
Principle #2: A child learns to regulate their own emotional arousal levels through co-regulation.
The next step in understanding emotional responses starts with a discussion about how a child learns to regulate their own systems as they mature. Regulation, as defined by Dr. Dan Siegel, is keeping the accelerator and brakes of arousal in balance. When a child is born they are completely dependent on an adult to help them modulate their arousal. They learn to regulate their own system through connection with a regulated caregiver. This co-regulation is what lays the foundation for self-regulation.
Imagine a baby that is hungry (uncomfortable and unsafe) and starts to cry. A caregiver comes (with its own system in a mobilization state) and picks up the baby and begins to rock and speaks to the baby in a calming fashion. The adult is using their regulated nervous system to regulate the baby’s nervous system. Over time the baby begins to learn how to regulate their own bodies.
It is important to note that if a child does not experience the presence of a regulated adult during early development, it delays its ability to self-regulate. This is why children who experience disrupted relationships early in life often struggle with social-emotional behavior. In blogs to come I will address further implications of trauma on a child.
Principal # 3 Connection is a biological Imperative
As humans, we are always seeking connection. It is how we are wired in our brains. A child needs connection to regulate their physiological being. It is in the presence of a connected caregiver that a child can grow and develop. When a child is operating in their window of tolerance (tolerating stress without freaking out), they are available for and desire connection. One of the challenges of a child who has experienced toxic stress or has sensory processing challenges is that the very connection they need is perceived as threatening. This is exhausting for them and can lead to challenging behaviors.
This is where the importance of being a regulated caregiver who can come alongside a child and BE the embodiment of regulation for them. They can ask in the moment:
Is this child regulated?
Is this child connected to me or to themselves?
Is this child feeling safe?
Here is where we really can dig deeper into behavior. We can look below the surface when a child is acting out. We can first determine if their physiological needs are being met. Are they hungry? Are they thirsty? Are they getting enough sleep?
We can prioritize being regulated ourselves in the moment so the child can experience co-regulation. Am I hungry? Am I getting enough sleep? Do I have enough margin? Check out my previous blogs on rest to learn more.
Consider your child’s lived experience. Are they over or under reactive to certain senses? If so, this could be impacting their ability to regulate and experience “felt safety.” (More on this to come!) Seek out an occupational therapist if you suspect your child struggles with this.
Stay tuned to my blog and my Instagram (@goskippingstone) for some examples of seeing what factors can lie beneath behaviors.
I hope that you are starting to see behavior in a new way. It takes time and practice to learn to respond to our children’s behavior with their nervous system in mind. It is not about being a perfect parent but it is about being on a journey of connection and helping your family move towards success in your everyday life.